Helen Frost, Health Director KWS
www.kwskeepingwomenstrong.com.au
May 24
7 min read
If you’re a woman, you will experience perimenopause and menopause – the timing, symptoms, and intensity may vary, but the transition is universal.
“Menopause isn’t an ending — it’s a powerful new beginning. A time to rise stronger, wiser, and fully in tune with your body.”
It’s a natural phase of life, not a malfunction—and with the right support, you can navigate it with strength, clarity, and confidence.
PERIMENOPAUSE is the transitional phase before menopause, when a woman’s hormones—especially estrogen—begin to fluctuate. It typically starts in the 40s but can begin as early as the mid-30s and lasts anywhere from a few months to several years.
Common Symptoms:
- Irregular periods
- Hot flashes and night sweats
- Mood swings or anxiety
- Sleep issues
- Brain fog
- Weight gain, especially around the belly
- Changes in libido or vaginal dryness
Perimenopause ends when a woman has gone 12 consecutive months without a period.
MENOPAUSE is then officially reached—a natural life phase, typically between ages 45 and 55, marking the permanent end of menstrual cycles.
Common Symptoms:
- Hot flashes & night sweats
- Sleep disturbances
- Mood changes & irritability
- Weight gain & slower metabolism
- Vaginal dryness & low libido
- Memory issues & brain fog
- Joint pain & fatigue
Menopause is a normal transition—not a disease.
You can manage symptoms and thrive in this stage of life with the right:
- Hormonal support. Yes, it is safe as the up-to-date research findings show below.
- Lifestyle habit changes, and whole food nutrition
- Exercise in the form of strength training and cardio
- Sleep and positive mindfulness
Hormone Replacement Therapy (HRT) has been avoided by many women for years due to a flawed 2002 study that overstated its risks.
The 2002 WHI Menopause Study refers to a landmark clinical trial conducted as part of the Women’s Health Initiative (WHI) — one of the largest and most influential women’s health studies in history.
What Was the WHI Menopause Study?
- Full Name: Women’s Health Initiative (WHI) Hormone Therapy Trial
- Launched: 1991; Hormone Trial findings published in 2002
- Participants: Over 160,000 postmenopausal women, aged 50–79
- Focus Areas: Heart disease, breast and colorectal cancer, osteoporosis, and effects of hormone replacement therapy (HRT)
- The trial—specifically combined estrogen and progestin (CEE + MPA).
Conclusions which caused concern for women BUT have since been corrected:
- ↑ Breast cancer risk
- ↑ Heart disease, stroke, and blood clots
- ↓ Colorectal cancer and hip fractures (some benefits observed)
However, the study had major limitations.
The Impact on Women:
- Created widespread fear and confusion about hormone therapy (HRT)
- Millions of women who were having positive outcomes stopped using HRT
- Major shift in menopause treatment guidelines and medical practices
- Later analysis found age and timing are crucial: younger women (closer to menopause onset) may experience different risk/benefit profiles than older women
More recent research has re-evaluated and clarified those early conclusions.
- The 2023 Study That Reassessed WHI:
The 2023 study titled:
“Revisiting the Women’s Health Initiative Hormone Therapy Trials: 20 Years Later“
Published in Menopause: The Journal of the North American Menopause Society (NAMS)By: JoAnn E. Manson, MD, DrPH, and Andrew M. Kaunitz, MD
Key Findings from the 2023 Reassessment:
- HRT is safe and beneficial for many women, especially when started before age 60 or within 10 years of menopause onset.
- The initial breast cancer risk was overstated, especially for estrogen-only therapy, which actually showed a reduction in breast cancer risk in some groups.
- The type, timing, and delivery method of hormones matter significantly (e.g., transdermal estrogen and bioidentical progesterone have different risk profiles than oral/synthetic options).
- HRT provides clear benefits for vasomotor symptoms (hot flashes), bone health, and quality of life.
Bottom Line:
The 2023 review did not “debunk” the WHI in the sense of proving it false, but rather corrected misinterpretations and placed its findings in proper context using 20 years of follow-up data and newer studies.
Further advocacy and study since 2023 have provided newer research showing that HRT is safe and effective for many women—especially when started near the onset of menopause.
- Latest 2025 Findings and GUIDELINES on HRT
Full Guidelines
2025 guidelines from The North American Menopause Society (NAMS)
- Timing Matters
New evidence shows that HRT started before age 60 or within 10 years of menopause onset is safe for many women and can even offer protective benefits against heart disease and osteoporosis.
- Type of Hormone Therapy
– The WHI study used a specific combination of hormones—synthetic progestin (MPA) and oral conjugated equine estrogen (CEE)—which are not the most commonly prescribed forms of HRT today.
– Newer forms, such as bioidentical hormones and transdermal (patch or gel) estrogen, carry less risk and be better tolerated.
- Breast Cancer Risk Is Small and Context-Dependent
– Later analyses of WHI data show the increased risk of breast cancer was very small, and mostly associated with long-term combined HRT use (rarely used estrogen + synthetic progestin).
– Estrogen-only therapy (for women without a uterus) showed no significant increase—and even a reduction—in breast cancer risk in some groups.
- Benefits Often Outweigh Risks for Symptomatic Women
– Current guidelines from groups like The North American Menopause Society (NAMS) and The Endocrine Society support the use of HRT for symptom relief and long-term health.
Key Takeaway:
HRT is not the universal threat it was once thought to be. For many women, it’s a safe and effective option—especially when tailored to their personal health history and started at the right time.
Why Estrogen Still Matters—Even Without Symptoms
Even if you’re not dealing with hot flashes, night sweats, or mood swings, estrogen plays critical roles in your long-term health. After menopause, your body produces far less estrogen—and that can silently affect several systems.
Risks associated with a decline and Low Estrogen After Menopause:
- Bone Loss & Osteoporosis
Low estrogen weakens bones, increasing the risk of fractures—especially in the hips, spine, and wrists, even if you feel fine now.
- Heart Disease
Estrogen helps protect blood vessels. Its decline can raise LDL (“bad”) cholesterol and increase the risk of heart disease, the #1 cause of death in women over 50.
- Brain Function and Cognitive Changes
Estrogen influences memory, mood, and cognitive sharpness. Even without symptoms, lower estrogen levels are linked to brain fog, memory decline, and a higher dementia risk over time.
- Vaginal & Urinary Changes
Thinning vaginal tissues, dryness, painful intercourse, and more frequent UTIs can occur.
Estrogen helps maintain vaginal tissue, elasticity, and bladder function. These issues may start subtly but often worsen over time without treatment—even without early symptoms.
- Mood Swings & Depression
Estrogen influences neurotransmitters like serotonin; its drop may affect mood and emotional well-being.
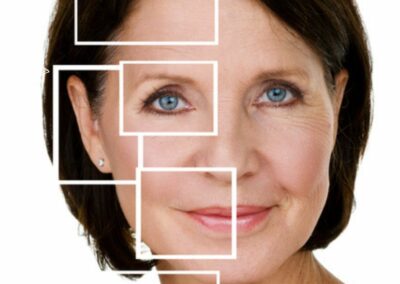
- Skin Aging & Elasticity Loss
Estrogen helps maintain collagen and skin hydration, so low levels can accelerate skin thinning and wrinkling.
Bottom Line:
You don’t need symptoms to benefit from estrogen support. HRT may still help protect your bones, brain, heart, and quality of life long-term. Talk to a healthcare provider who stays current with the latest research to decide if it’s right for you.
Benefits of Estrogen (or Estrogen + Progestin) Therapy
Relief from Menopausal Symptoms
- Reduces hot flashes and night sweats
- Improves sleep quality
- Eases mood swings, anxiety, and irritability
- Reduces vaginal dryness and painful intercourse
- Improves urinary tract health
Protects Bone Health
- Helps prevent bone loss and osteoporosis
- Lowers risk of fractures, especially in the hip and spine
Supports Heart Health
- May lower risk of coronary heart disease when started before age 60 or within 10 years of menopause
Supports Brain Health
- Potentially reduces brain fog and may help with cognitive clarity
- Research is ongoing on the connection to dementia prevention when started early
Improves Metabolism & Body Composition
- Helps reduce central weight gain (visceral fat) and maintain lean muscle mass
- May improve insulin sensitivity and cholesterol levels
Note:
- Combined therapy (estrogen + progestin) is used for women with a uterus to protect against endometrial cancer.
- Women without a uterus can take estrogen alone.
Key Research Findings on increased Visceral Fat (belly fat) After Menopause
- Hormonal Changes Drive Fat Redistribution
- A 2009 study in Journal of Clinical Endocrinology & Metabolism showed that the drop in estrogen, not just aging alone, directly contributes to increased visceral fat.
- Estrogen helps regulate fat distribution. After menopause, fat shifts from the hips and thighs to the abdomen.
- Increased Risk of Metabolic Disease
- Visceral fat is more metabolically active than subcutaneous fat and is linked to:
- Insulin resistance
- Type 2 diabetes
- Heart disease
- Inflammation and oxidative stress
- The Study of Women’s Health Across the Nation (SWAN) confirmed that visceral fat increases independent of BMI, meaning even women who don’t gain weight overall may accumulate harmful belly fat.
- HRT May Help Limit Visceral Fat
- Research (e.g., Menopause, 2012) shows that estrogen therapy may reduce visceral fat accumulation and improve insulin sensitivity when started early in the menopause transition.
Takeaway:
After menopause, visceral fat becomes a major health concern—even if overall body weight stays the same.
Estrogen loss, reduced physical activity, inadequate nutrition for the aging body and slower metabolism all contribute.
Keys to managing VISCERAL FAT
Lifestyle and Medical interventions
- Resistance training and regular functional movement
- A high-protein whole food eating plan and healthy lifestyle habits
- HRT
FINAL WORDS to ALL WOMEN
You are the expert on your body.
If your doctor isn’t current on the latest research about hormone therapy, that’s not a signal to stay silent—it’s a call to speak up and self-advocate knowing you have the backing of research and many up-to-date health professionals around the world.
Science has evolved.
We now know that HRT, when used appropriately, is safe and effective for many women.
It’s okay to ask questions, bring articles, or request a referral if the doctor is not up to speed.
A second opinion is not a betrayal—it’s self-respect.
Your symptoms are real. Your quality-of-life matters.
YOU deserve evidence-based care, not outdated fear.
“You’ve navigated life — now step into your prime with knowledge, action, purpose, strength, power, and pride.”
YOU deserve to be a ‘Stronger Woman’ with the correct SELF CARE.












0 Comments